ONLINE EDITION PAIN
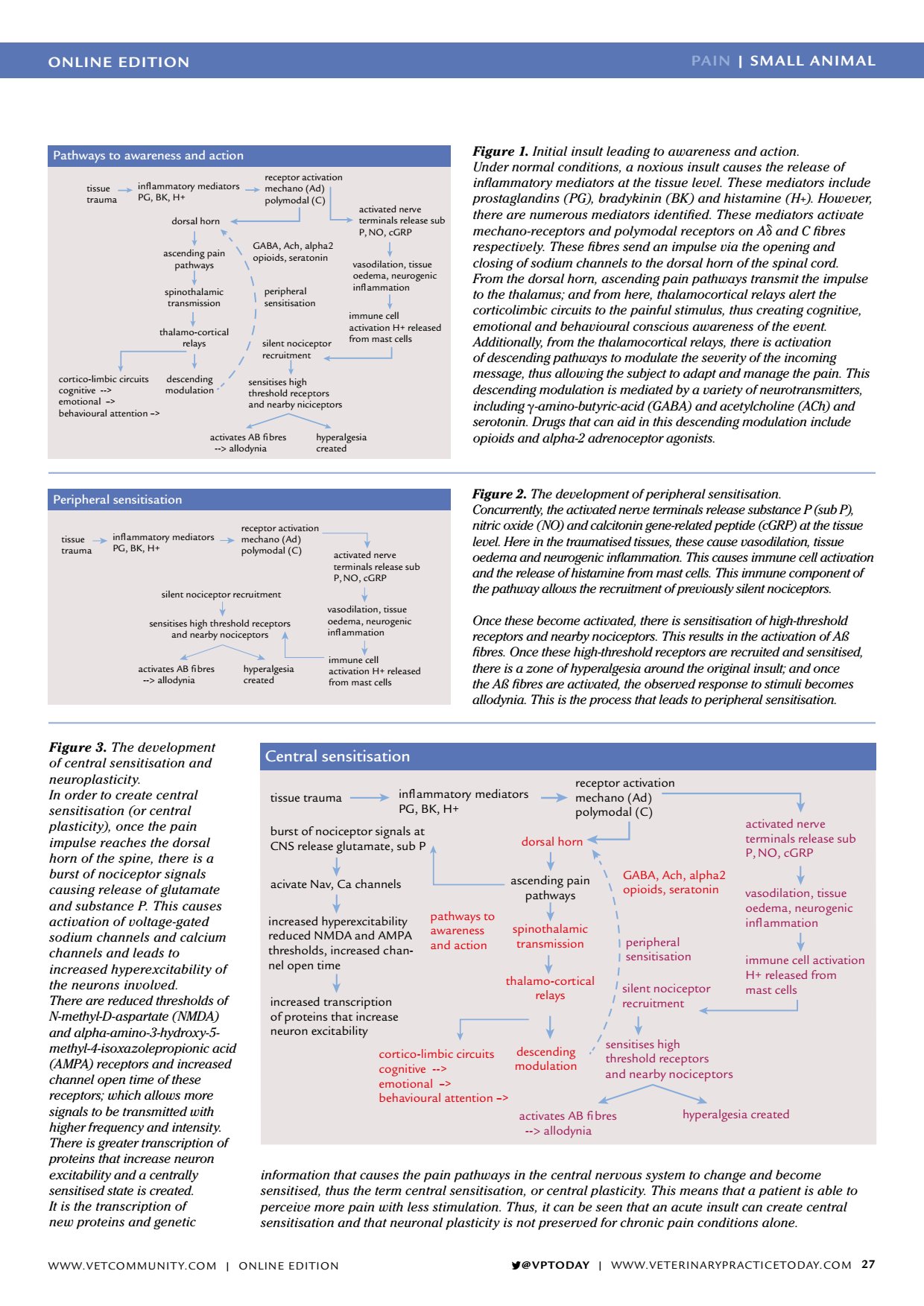
ONLINE EDITION PAIN | SMALL ANIMAL VPTODAY | WWW.VETERINARYPRACTICETODAY.COM 27 Pathways to awareness and action tissue trauma inflammatory mediators PG, BK, H+ receptor activation mechano (Ad) polymodal (C) dorsal horn ascending pain pathways spinothalamic transmission thalamo-cortical relays descending modulation cortico-limbic circuits cognitive --> emotional > behavioural attention > GABA, Ach, alpha2 opioids, seratonin activated nerve terminals release sub P, NO, cGRP vasodilation, tissue oedema, neurogenic inflammation immune cell activation H+ released from mast cells peripheral sensitisation silent nociceptor recruitment sensitises high threshold receptors and nearby niciceptors activates AB fibres -- > allodynia hyperalgesia created Figure 1. Initial insult leading to awareness and action. Under normal conditions, a noxious insult causes the release of inflammatory mediators at the tissue level. These mediators include prostaglandins (PG), bradykinin (BK) and histamine (H+). However, there are numerous mediators identified. These mediators activate mechano-receptors and polymodal receptors on A δ and C fibres respectively. These fibres send an impulse via the opening and closing of sodium channels to the dorsal horn of the spinal cord. From the dorsal horn, ascending pain pathways transmit the impulse to the thalamus; and from here, thalamocortical relays alert the corticolimbic circuits to the painful stimulus, thus creating cognitive, emotional and behavioural conscious awareness of the event. Additionally, from the thalamocortical relays, there is activation of descending pathways to modulate the severity of the incoming message, thus allowing the subject to adapt and manage the pain. This descending modulation is mediated by a variety of neurotransmitters, including γ -amino-butyric-acid (GABA) and acetylcholine (ACh) and serotonin. Drugs that can aid in this descending modulation include opioids and alpha-2 adrenoceptor agonists. Figure 2. The development of peripheral sensitisation. Concurrently, the activated nerve terminals release substance P (sub P), nitric oxide (NO) and calcitonin gene-related peptide (cGRP) at the tissue level. Here in the traumatised tissues, these cause vasodilation, tissue oedema and neurogenic inflammation. This causes immune cell activation and the release of histamine from mast cells. This immune component of the pathway allows the recruitment of previously silent nociceptors. Once these become activated, there is sensitisation of high-threshold receptors and nearby nociceptors. This results in the activation of Aß fibres. Once these high-threshold receptors are recruited and sensitised, there is a zone of hyperalgesia around the original insult; and once the Aß fibres are activated, the observed response to stimuli becomes allodynia. This is the process that leads to peripheral sensitisation. Central sensitisation tissue trauma inflammatory mediators PG, BK, H+ receptor activation mechano (Ad) polymodal (C) dorsal horn ascending pain pathways spinothalamic transmission thalamo-cortical relays descending modulation cortico-limbic circuits cognitive --> emotional > behavioural attention > GABA, Ach, alpha2 opioids, seratonin activated nerve terminals release sub P, NO, cGRP vasodilation, tissue oedema, neurogenic inflammation immune cell activation H+ released from mast cells peripheral sensitisation silent nociceptor recruitment sensitises high threshold receptors activates AB fibres -- > allodynia hyperalgesia created increased transcription of proteins that increase neuron excitability increased hyperexcitability reduced NMDA and AMPA thresholds, increased chan- nel open time acivate Nav, Ca channels burst of nociceptor signals at CNS release glutamate, sub P pathways to awareness and action Figure 3. The development of central sensitisation and neuroplasticity. In order to create central sensitisation (or central plasticity), once the pain impulse reaches the dorsal horn of the spine, there is a burst of nociceptor signals causing release of glutamate and substance P. This causes activation of voltage-gated sodium channels and calcium channels and leads to increased hyperexcitability of the neurons involved. There are reduced thresholds of N-methyl-D-aspartate (NMDA) and alpha-amino-3-hydroxy-5- methyl-4-isoxazolepropionic acid (AMPA) receptors and increased channel open time of these receptors; which allows more signals to be transmitted with higher frequency and intensity. There is greater transcription of proteins that increase neuron excitability and a centrally sensitised state is created. It is the transcription of new proteins and genetic Peripheral sensitisation tissue trauma inflammatory mediators PG, BK, H+ receptor activation mechano (Ad) polymodal (C) activated nerve terminals release sub P, NO, cGRP vasodilation, tissue oedema, neurogenic inflammation immune cell activation H+ released from mast cells silent nociceptor recruitment sensitises high threshold receptors and nearby nociceptors activates AB fibres -- > allodynia hyperalgesia created information that causes the pain pathways in the central nervous system to change and become sensitised, thus the term central sensitisation, or central plasticity. This means that a patient is able to perceive more pain with less stimulation. Thus, it can be seen that an acute insult can create central sensitisation and that neuronal plasticity is not preserved for chronic pain conditions alone. and nearby nociceptors WWW.VETCOMMUNIT Y.COM | ONLINE EDITION