Clinical signs Diagnosis
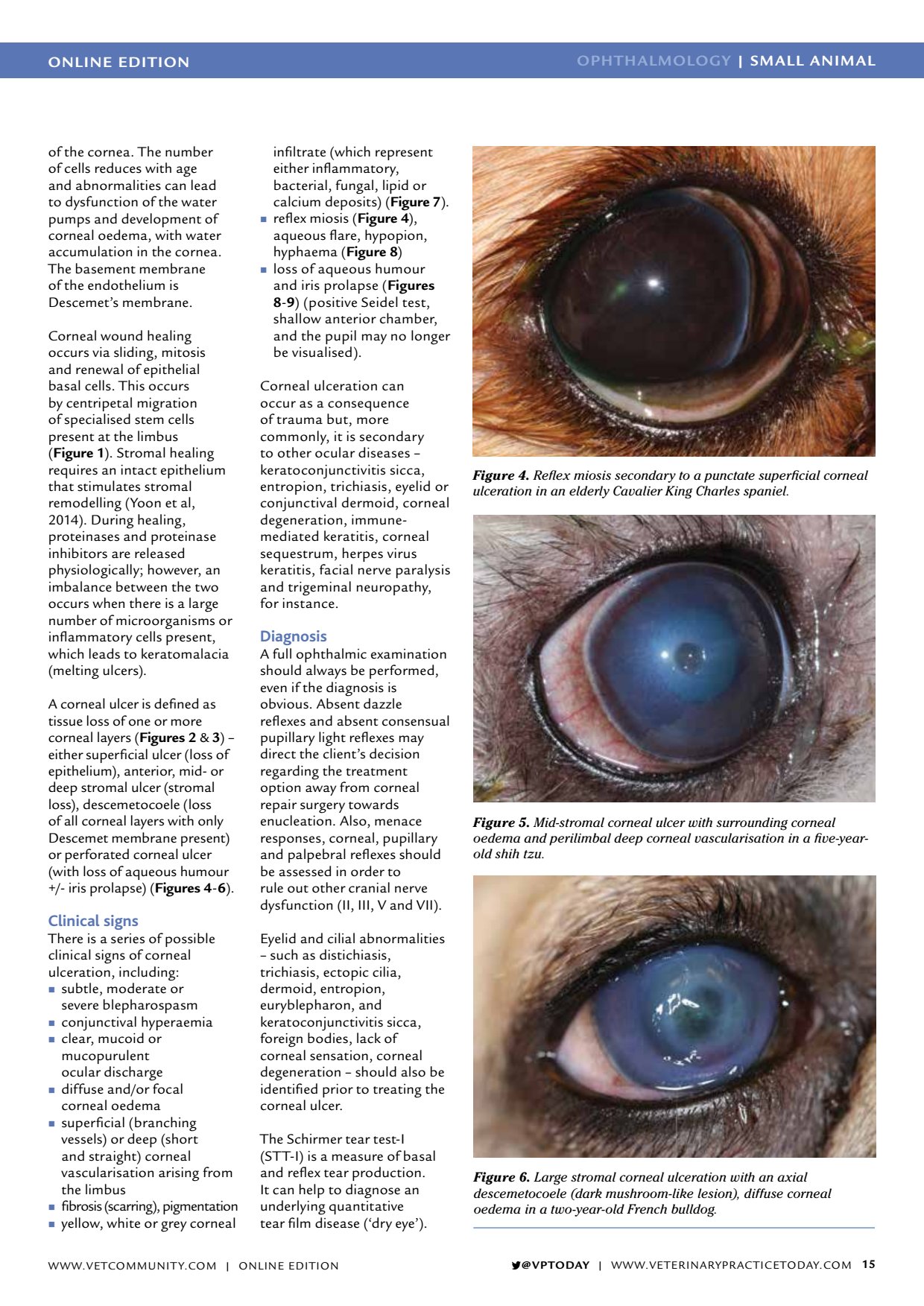
ONLINE EDITION OPHTHALMOLOGY | SMALL ANIMAL VPTODAY | WWW.VETERINARYPRACTICETODAY.COM 15 of the cornea. The number of cells reduces with age and abnormalities can lead to dysfunction of the water pumps and development of corneal oedema, with water accumulation in the cornea. The basement membrane of the endothelium is Descemets membrane. Corneal wound healing occurs via sliding, mitosis and renewal of epithelial basal cells. This occurs by centripetal migration of specialised stem cells present at the limbus ( Figure 1 ). Stromal healing requires an intact epithelium that stimulates stromal remodelling (Yoon et al, 2014). During healing, proteinases and proteinase inhibitors are released physiologically; however, an imbalance between the two occurs when there is a large number of microorganisms or inflammatory cells present, which leads to keratomalacia (melting ulcers). A corneal ulcer is defined as tissue loss of one or more corneal layers ( Figures 2 & 3 ) either superficial ulcer (loss of epithelium), anterior, mid- or deep stromal ulcer (stromal loss), descemetocoele (loss of all corneal layers with only Descemet membrane present) or perforated corneal ulcer (with loss of aqueous humour +/- iris prolapse) ( Figures 4 - 6 ). Clinical signs There is a series of possible clinical signs of corneal ulceration, including: subtle, moderate or severe blepharospasm conjunctival hyperaemia clear, mucoid or mucopurulent ocular discharge diffuse and/or focal corneal oedema superficial (branching vessels) or deep (short and straight) corneal vascularisation arising from the limbus fibrosis (scarring), pigmentation yellow, white or grey corneal infiltrate (which represent either inflammatory, bacterial, fungal, lipid or calcium deposits) ( Figure 7 ). reflex miosis ( Figure 4 ), aqueous flare, hypopion, hyphaema ( Figure 8 ) loss of aqueous humour and iris prolapse ( Figures 8 - 9 ) (positive Seidel test, shallow anterior chamber, and the pupil may no longer be visualised). Corneal ulceration can occur as a consequence of trauma but, more commonly, it is secondary to other ocular diseases keratoconjunctivitis sicca, entropion, trichiasis, eyelid or conjunctival dermoid, corneal degeneration, immune- mediated keratitis, corneal sequestrum, herpes virus keratitis, facial nerve paralysis and trigeminal neuropathy, for instance. Diagnosis A full ophthalmic examination should always be performed, even if the diagnosis is obvious. Absent dazzle reflexes and absent consensual pupillary light reflexes may direct the clients decision regarding the treatment option away from corneal repair surgery towards enucleation. Also, menace responses, corneal, pupillary and palpebral reflexes should be assessed in order to rule out other cranial nerve dysfunction (II, III, V and VII). Eyelid and cilial abnormalities such as distichiasis, trichiasis, ectopic cilia, dermoid, entropion, euryblepharon, and keratoconjunctivitis sicca, foreign bodies, lack of corneal sensation, corneal degeneration should also be identified prior to treating the corneal ulcer. The Schirmer tear test-I (STT-I) is a measure of basal and reflex tear production. It can help to diagnose an underlying quantitative tear film disease (dry eye). Figure 4. Reflex miosis secondary to a punctate superficial corneal ulceration in an elderly Cavalier King Charles spaniel. Figure 5. Mid-stromal corneal ulcer with surrounding corneal oedema and perilimbal deep corneal vascularisation in a five-year- old shih tzu. Figure 6. Large stromal corneal ulceration with an axial descemetocoele (dark mushroom-like lesion), diffuse corneal oedema in a two-year-old French bulldog. WWW.VETCOMMUNIT Y.COM | ONLINE EDITION